Birth Control Methods
There are two main tools for avoiding unplanned pregnancy: abstinence and birth control (contraception). Below you will find more information about both abstinence and birth control.
There are five main types of contraception: long-acting reversible contraception (LARC), short-acting hormonal methods, barrier methods, emergency contraception, and sterilization. Barrier methods is covered on the Barrier Methods page.
In addition, check out this video going over different types of contraception.
Not having sex is the only way to guarantee you won’t get a sexually transmitted infection (STI) or have an unplanned pregnancy. This means avoiding all sexual contact, including oral sex, anal sex, vaginal sex, and genital-to-genital touching. Sound tough? It is, but if you think it’s the right thing for you, being prepared can help. If you choose to abstain, here are some tips on sticking to your decision:
- Remind yourself why you chose to wait. Think about the consequences (e.g., pregnancy, STIs) of sex. If you don’t have a clear plan for avoiding STIs and unplanned pregnancy (condoms and a reliable form of birth control), you aren’t ready to have sex.
- The heat of the moment isn’t the right time to reconsider your decision. Stick to your decision until you can think about it clearly. Remember, not everyone is “doing it”.
- Talk to people you trust about your decision to not have sex and lean on them for support.
- Be straightforward and clear about your decision and your limits with your partner. Talk about your decision with them before you get into a sexual situation.
- Avoid putting yourself in uncomfortable situations that will make it difficult to stick to your decision to wait.
- Consider avoiding alcohol and drugs. Alcohol and drugs can make it much harder to stick to any decision, especially abstinence.
LARCs are the most effective birth control methods that can work for years and are also reversible, meaning you can stop using them at any time you’d like. LARCs do not protect against STIs, so make sure to wear a condom! There are two types of LARCs: intrauterine devices (IUDs) and implants.
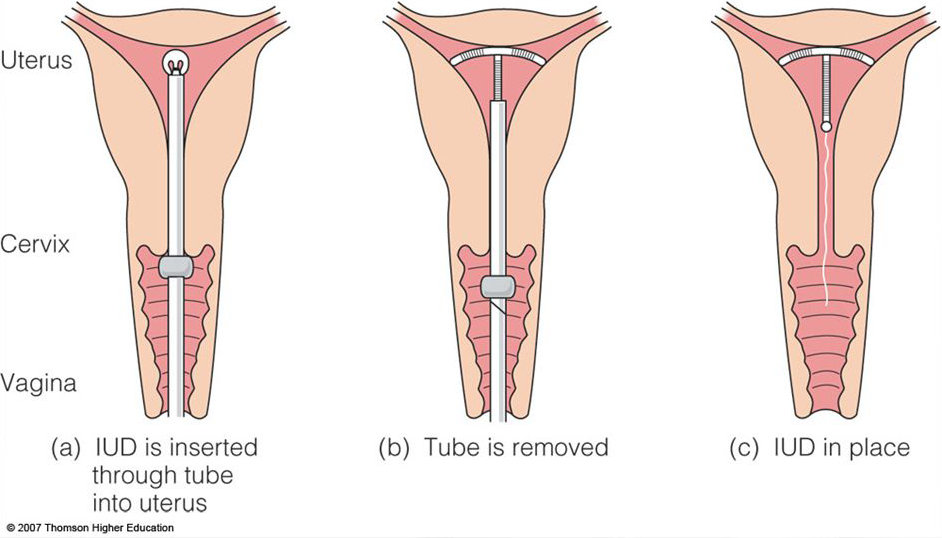
Intrauterine Devices (IUDs)
An IUD is a small and flexible T-shaped device that is inserted into the uterus. When placed properly, neither you nor your partner should be able to feel the IUD. You can have your IUD removed by a healthcare provider at any time if you decide you are ready to become pregnant or want to use a different method. IUDs are effective at preventing pregnancy more than 99% of the time. There are five types of IUDs available:
- Skyla. The smallest of the IUDs, which lasts up to 3 years.
- Kyleena. Lasts up to 5 years.
- Liletta. Lasts up to 7 years.
- Mirena. Lasts up to 7 years.
- Paragard. Lasts up to 10 years. The Paragard IUD is a hormone free birth control method made of copper that can also be used for emergency contraception (EC) up to 5 days after having unprotected sex. It prevents both egg fertilization and implantation. Paragard is effective regardless of a woman’s weight.
If you’re interested in using an IUD, visit the Find a Doctor page to find a healthcare provider near you who can provide it.
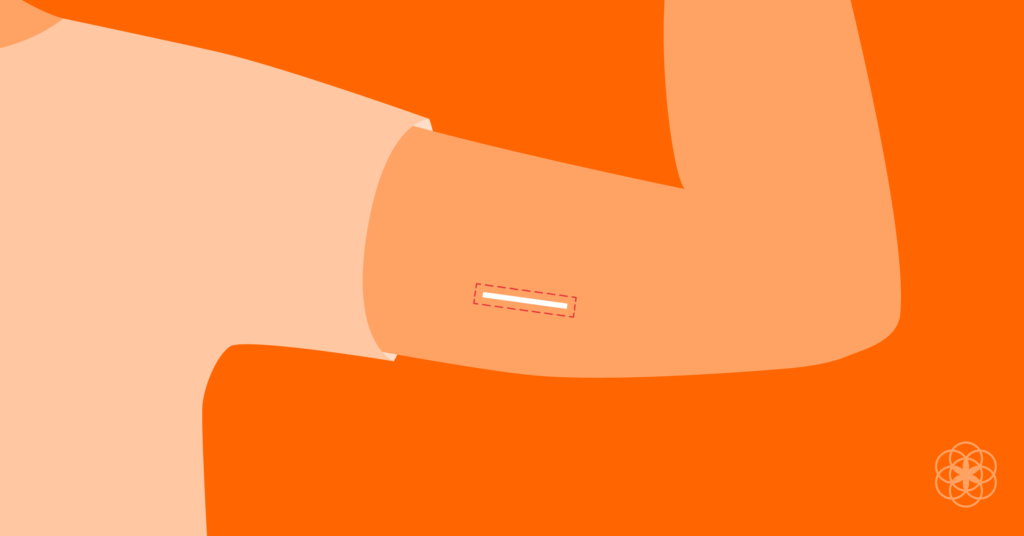
Implants (Nexplanon)
An implant is a small rod about the size of a matchstick that is inserted in your upper arm just below the skin. This implant can be felt when you press your skin, but it can barely be seen. This type of birth control lasts up to 3 years and can be removed by a healthcare provider at any time if you decide you are ready to become pregnant or want to use a different method. The implant is more than 99% effective at preventing pregnancy.
If you’re interested in using an implant, visit the Find a Doctor page to find a healthcare provider near you who can provide it.
These birth control methods contain hormones that prevent ovulation (the release of an ovum/egg from the ovaries) and/or affect the mucus around the cervix to be unfriendly to sperm. IUDs (except Paragard) and implants also contain hormones, but these methods last for a shorter period than LARCs. There are four types of hormonal methods described below.
The Shot (Depo-Provera)
This is the contraceptive shot. Depo-Provera, also known as Depo, is an injection that is given every 3 months. This type of birth control must be administered by a healthcare provider and is 94% effective at preventing pregnancy.
If you’re interested in getting Depo-Provera, visit the Find a Doctor page to find a healthcare provider near you who can provide it.

Birth Control Pills (Oral Contraceptives)
Birth control pills are taken by mouth daily at the same time. There are many different types of pills available, each with different names, amounts of medication in them, and side effects. Your healthcare provider can help you to determine which pill is best for you. Oral contraceptives are effective at preventing pregnancy 91% of the time.
If you’re interested in using birth control pills, visit the Find a Doctor page to find a healthcare provider near you who can provide it.
Vaginal Ring (NuvaRing)
The vaginal ring is a thin, flexible ring about 2 inches across. It is inserted into your vagina. When inserted properly, neither you nor your partner can feel it. The ring stays in for 3 weeks and comes out for 1 week, then a new ring must be inserted. This process must be repeated every month. This type of birth control is effective 91% of the time.
If you’re interested in using a vaginal ring, visit the Find a Doctor page to find a healthcare provider near you who can provide it.

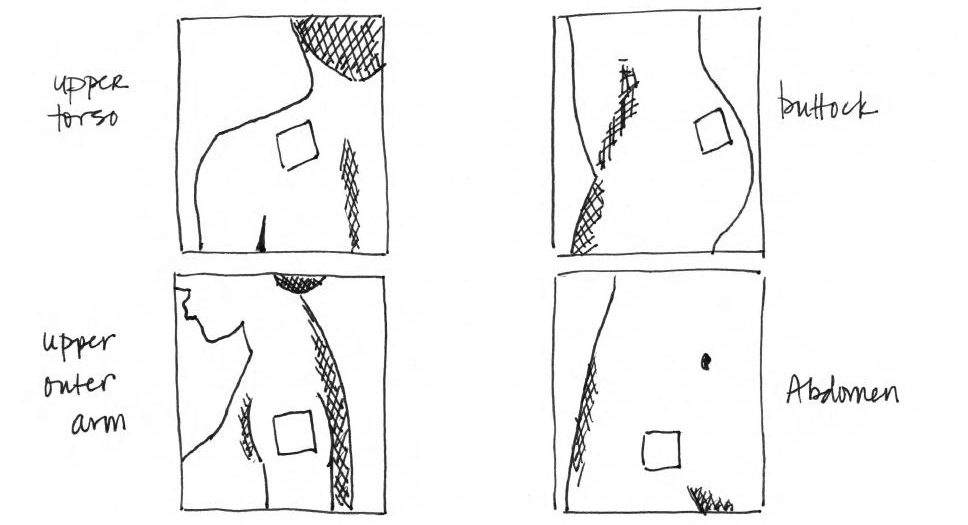
The Patch (Ortho Evra)
The patch is a thin piece of plastic that resembles a square Band-Aid. The sticky part of the patch is placed on your skin. It’s worn for a week and then replaced with a new one. During the fourth week, you do not wear a patch and will get your period. This type of birth control is effective 91% of the time.
If you’re interested in using the patch, visit the Find a Doctor page to find a healthcare provider near you who can provide it.
Barrier methods are a type of birth control that are different from the ones described on this page because they are barriers that keep sperm from entering a uterus and fertilizing an egg during sexual intercourse. They can also help in protecting against the spread of STIs. Learn about them on the Barrier Methods page!
Emergency contraceptives are a type of birth control that prevents pregnancy after sex. You should use ECs right away if you didn’t use birth control, missed pills, forgot to change your ring or patch, or if your condom broke during sex. ECs do not end pregnancies, but rather prevent conception. There are three main types of ECs: Plan B One-Step, Ella, and Paragard IUD.
Plan B One-Step
Plan B is a hormone pill, similar to birth control pills that can prevent unplanned pregnancy after unprotected intercourse. It should be taken as soon as possible after intercourse but is effective in preventing unwanted pregnancy when taken within the first 3 days after sex. It has decreased effectiveness if taken up to 5 days after having sex. However, it’s not as effective for women over 175 lbs.
If you need Plan B, it should be available over the counter (without a prescription) at your local pharmacy. The pharmacist can help you find it.
Ella
Ella is a hormone pill, similar to birth control pills that can prevent unplanned pregnancy after unprotected intercourse. It should be taken as soon as possible after intercourse and can be taken be up to 5 days after having sex. It is more effective than Plan B for women weighing 175 lbs and greater. A prescription is needed for Ella.
If you’re interested in using Ella, visit the Find a Doctor page to find a healthcare provider near you who can provide it.
Paragard IUD
Paragard is a hormone free birth control method that can also be used for EC up to 5 days after having unprotected sex. It prevents both egg fertilization and implantation and is effective regardless of a woman’s weight. You’ll need to see a healthcare provider to have Paragard inserted. The other great thing about Paragard is that it provides very reliable contraception for up to 10 years!
If you’re interested in using Paragard, visit the Find a Doctor page to find a healthcare provider near you who can provide it.

Sterilization is a permanent form of birth control that involves surgery to prevent sperm and an egg from meeting. There are two types of sterilization: tubal ligation and vasectomy.
Tubal Ligation
Tubal ligation is the female sterilization method. It’s also known as “tying tubes” because your fallopian tubes are tied or closed to prevent an egg from traveling down the tubes to reach the uterus or sperm from traveling up to reach an egg.
Vasectomy
A vasectomy is the male sterilization method. It prevents sperm from traveling to the penis and entering a vagina. This method is safer and more effective at preventing pregnancy than tubal ligation.
Withdrawal (Pulling Out)
Withdrawal is when you pull out your penis from the vagina before you ejaculate. This method must be done perfectly every time to prevent pregnancy, which is very difficult. Plus, withdrawal offers no STI protection. The best thing to do is to stick with condoms and one of the birth control methods listed above.
Fertility Awareness-Based Methods (FAMs)
This involves understanding your monthly fertility pattern to plan when you can get pregnant and avoid getting pregnant. Your fertility pattern is the following:
- Number of days that you’re fertile (able to get pregnant)
- Number of days that you’re infertile
- Days when fertility is unlikely, but possible
Lactational Amenorrhea Method (LAM)
The LAM is used when you’re breastfeeding and is a temporary method of birth control. You can use it only when all three of the following conditions are met:
- Amenorrhea (no menstruation) after giving birth,
- Fully or nearly fully breastfeeding, and
- It’s been less than 6 months since giving birth.
If any of the three conditions are not met, then you won’t be able to use this method and you should use another method described above to prevent pregnancy.
Outercourse
Outercourse is similar to abstinence, except some sexual activity may happen. This method does not involve vaginal sex or getting sperm in a vagina. Examples of outercourse include:
- Kissing
- Dry humping
- Anal sex
- Oral sex
If you decide to engage in outercourse, particularly anal or oral sex, there is a risk of contracting STIs, so make sure to also wear a condom.
Content reviewed by Shandhini Raidoo, MD, MPH, FACOG
Last Updated: September 25, 2020 by Phyllis Raquinio
Sources
- IUD Photo: Francke, T. (2019, October 17). Five Questions to Ask Your Doctor Before Getting an IUD. Retrieved July 22, 2020, from https://medtruth.com/articles/health-features/five-questions-iud/
- IUD Insertion Photo: Teen Health Source. (n.d.). What To Expect When Getting An IUD. Retrieved July 22, 2020, from http://teenhealthsource.com/blog/what-to-expect-when-getting-an-iud/
- Implant Photo: Bell, J. (2019, January 15). What it’s like to use a birth control implant. Retrieved July 22, 2020, from https://helloclue.com/articles/sex/what-it’s-like-to-use-a-birth-control-implant
- The Shot Photo: Bedsider. (2020, March). The Shot. Retrieved July 22, 2020, from https://www.bedsider.org/methods/the_shot
- Birth Control Pills Photo: Planned Parenthood. (n.d.). How to Use Birth Control Pills. Retrieved July 22, 2020, from https://www.plannedparenthood.org/learn/birth-control/birth-control-pill/how-do-i-use-the-birth-control-pill
- Vaginal Ring Photo: Miller, K. (2019, January 25). How to Insert NuvaRing So It Stays in Place. Retrieved July 22, 2020, from https://www.self.com/story/how-to-insert-nuvaring
- The Patch Photo: Cody, J. (2018, June 22). Let’s Talk About Family Planning – Part 2: Family Planning Options and How They Work. Retrieved July 22, 2020, from https://nashville.citymomsblog.com/lets-talk-family-planning-part-2-family-planning-options-work/
- Plan B One-Step Photo: Rovner, J. (2013, July 24). Plan B To Hit Shelves, Protected From Generics. Retrieved July 22, 2020, from https://www.npr.org/sections/health-shots/2013/07/24/205182187/plan-b-to-hit-shelves-protected-from-generics
- Ella Photo: Staiger, B. (2019, October 25). Ella: How Long Do Side Effects Of The Emergency Contraceptive Last? Retrieved July 22, 2020, from https://walrus.com/questions/how-long-do-ella-side-effects-last
- Paragard IUD Photo: Couzin-Frankel, J. (2011, July 15). Contraceptive Comeback: The Maligned IUD Gets a Second Chance. Retrieved July 22, 2020, from https://www.wired.com/2011/07/ff_iud/